Telephonic Case Management in Workers’ Compensation

TODAY, HEALTHCARE COSTS CONTINUE TO RISE IN THE WORKERS’ COMPENSATION INDUSTRY. PAYERS ARE LOOKING FOR METHODS TO PROVIDE COST-EFFECTIVE OUTCOMES. ACCORDING TO THE U.S. BUREAU OF LABOR STATISTICS, THERE WERE NEARLY 2.9 MILLION NONFATAL WORKPLACE INJURIES AND ILLNESSES REPORTED IN 2015[1]. CASE MANAGEMENT MAY HELP AVOID UNNECESSARY MEDICAL SPENDING BY DECREASING INEFFECTIVE CARE, REDUCING HOSPITAL READMISSIONS, AND RETURNING EMPLOYEES TO WORK. WITHIN THE FIELD OF CASE MANAGEMENT, TELEPHONIC CASE MANAGEMENT CAN PROVIDE UNIQUE BENEFITS.
Telephonic Case Management
Telephonic Case Management (TCM) provides benefits relative to cost-effective early intervention, removal of geographic restrictions, and reduced travel and wait time costs. In TCM, the coordination of care is handled by a nurse telephonically. The use of a telephone for managing a claimant’s file can bring substantial benefits.
One of the benefits obtained by utilizing TCM is the removal of geographic restrictions associated with a nurse’s field office. Working telephonically allows a nurse to cover multiple files for injured workers in different locations or files with medical activity spanning different areas. For example, on some occasions injured workers move during their time out of work and physicians may need to be consulted in different areas. A telephonic nurse can easily accomplish this without the complications of travel. In addition, the adjuster benefits from the use of TCM because they have the convenience of working with one nurse on multiple cases that require case management services, regardless of the claimant’s location. This allows the adjuster and case manager to gain familiarity and work more efficiently and effectively together. By removing the need for travel and face to face interaction, the nurse can increase their productivity in managing the claimant’s file.
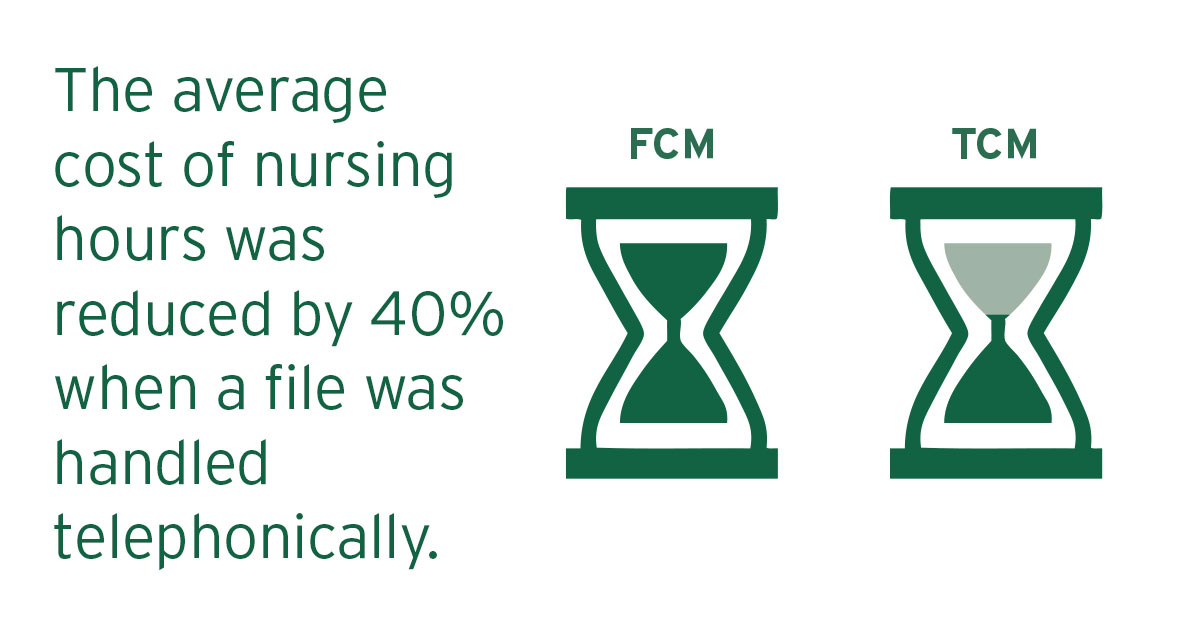
TCM services can reduce costs compared to traditional Field Case Management (FCM) by eliminating expenses associated with travel, appointments, and wait time. The nurse can monitor the file by reviewing the medical reports completed by the physician following an appointment and discern if a telephonic consult is needed. In a recent internal study of 2,000 active files, the average cost of nursing hours was reduced by 40% when a file was handled by TCM as opposed to FCM. The cost savings associated with this service are substantial and can be performed while meeting the objectives established on the file.
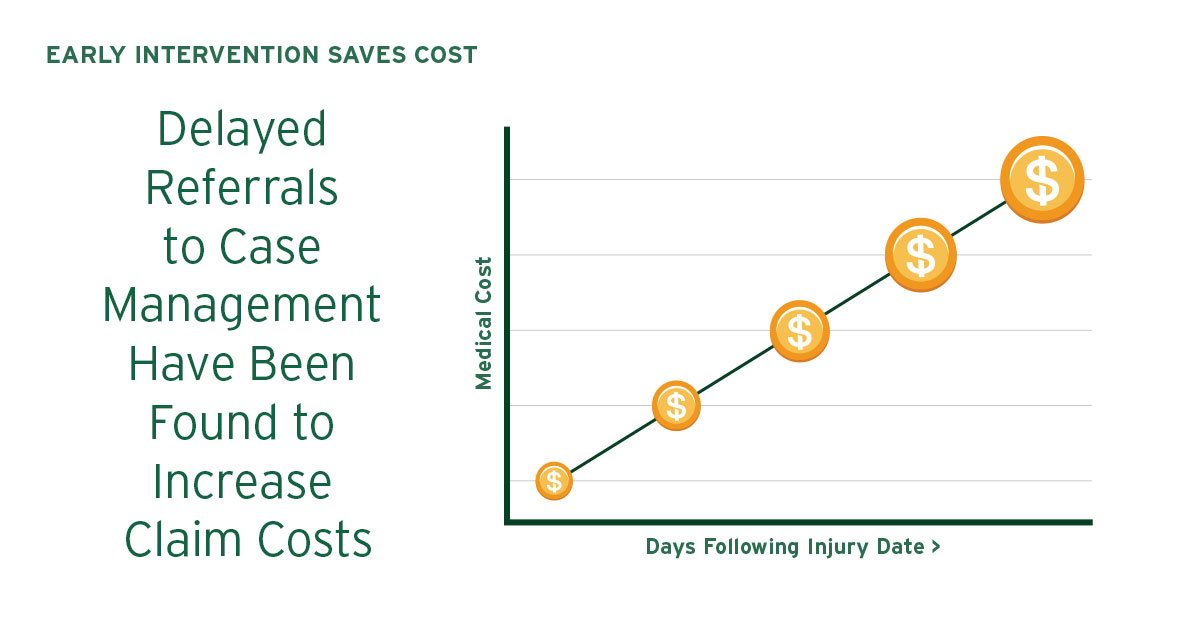
TCM can be used at different points throughout the duration of the claim. In order to obtain the best possible results, an early intervention strategy should be put in place to manage work-related injuries. To address this challenge, many employers and third party administrators are utilizing TCM nurses. Referencing treatment protocols, TCM nurses systematically identify the appropriate level of care and provide an early intervention strategy, offering medical expertise and an injury triage to set claims on the right track from the beginning. Cost savings are maximized when case management needs are identified early in the process.
When is Field Case Management a better fit?
TCM nurses and adjusters are trained to identify instances where the benefits of FCM should be applied. There are a number of indicators for when a file would benefit from the additional expenses associated with FCM.
- Catastrophic
- Anticipated long-term care
- Inadequate communication among the involved parties
- Physician’s treatment plan is outside the evidence-based medical guidelines (i.e. Official Disability Guidelines)
These issues may not require a file to be managed by a FCM nurse, however can benefit from a field task assignment. With a field task assignment, a specific goal can be met while under the management of the TCM nurse. There is a level of discretion in regards to whether a file should be managed by FCM or TCM.
Field Case Management is a necessary and valuable tool that should not be underutilized, as there are instances when having the nurse on site can make a difference.
IN SOME CASES, CLAIMANTS MAY NEED A NURSE TO ATTEND APPOINTMENTS BECAUSE THEY MAY BE APPREHENSIVE IN REGARDS TO TREATMENT OR MAY NOT KNOW THE RIGHT QUESTIONS TO ASK THE PHYSICIAN. IN THESE CASES, BY ATTENDING THE PHYSICIAN APPOINTMENT WITH THE CLAIMANT, THE CASE MANAGER CAN KEEP THE OBJECTIVES IN MIND AND ADVOCATE FOR THE CLAIMANT.

Case Study
A 59-year-old mechanic was climbing on an elevated conveyor belt when he hit his head on a beam and fell twenty feet onto a concrete foundation. The injured worker suffered multiple injuries, including closed head fractures, hemorrhages, back, shoulder, and knee injuries. On the date of injury, the claimant was airlifted to a local hospital where he remained in ICU for over one week. Initially, due to the details of the injury, a FCM was assigned to manage the catastrophic file. Over the course of several months, the injured worker had numerous hospital readmissions that involved various surgical procedures and diagnostic testing. Due to our knowledge in handling catastrophic claims and being a much needed cost-effective option, a TCM was assigned to coordinate the ongoing medical needs associated with the claimant’s rehabilitation and long-term care. The injured worker is under the continuous care of nine specialists. TCM effectively manages the file telephonically and collaborates with all specialists, therapists, and family members, as well as the carrier, providing high quality care to the injured worker.
Conclusion
Case Management is a valuable service that provides extensive benefits to the injured worker and the payer. Determining the appropriateness of assigning a case manager to a file is an important aspect of managing the costs associated with any claim. Once the need for case management is determined to be suitable for a file, utilizing TCM can benefit all parties involved by providing cost-effective early intervention, removal of geographic restrictions, and reduced travel costs. TCM is a favorable solution for managing a claimant’s file while delivering optimal care.
ADDITIONAL RESOURCES:
This whitepaper was prepared by Carlisle Medical in collaboration with staff Nurse Case Manager Supervisor, Louise Moore, RN. Carlisle Medical has over 30 years of experience as a leader in healthcare cost containment to the workers’ compensation industry. Our company can help insurance carriers, third party administrators, and employers significantly reduce their workers’ compensation costs. Our experienced staff of licensed pharmacists and nurses can assist companies with injuries ranging from minor to catastrophic.
REFERENCES:
[1] “Employer-Reported Workplace Injury and Illness Summary.” U.S. Bureau of Labor Statistics. U.S. Bureau of Labor Statistics, 27 Oct. 2016. Web. 21 June 2017.