Prescription Reviews Utilizing Nurse/Physician Consultation Yield More Favorable Claim Outcomes

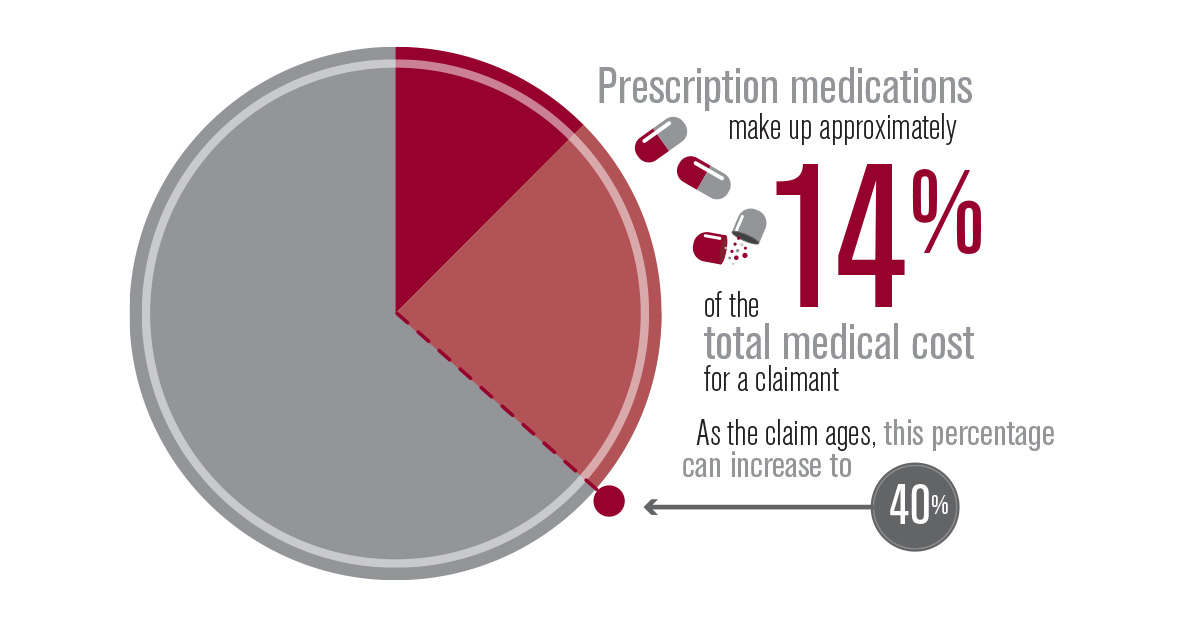
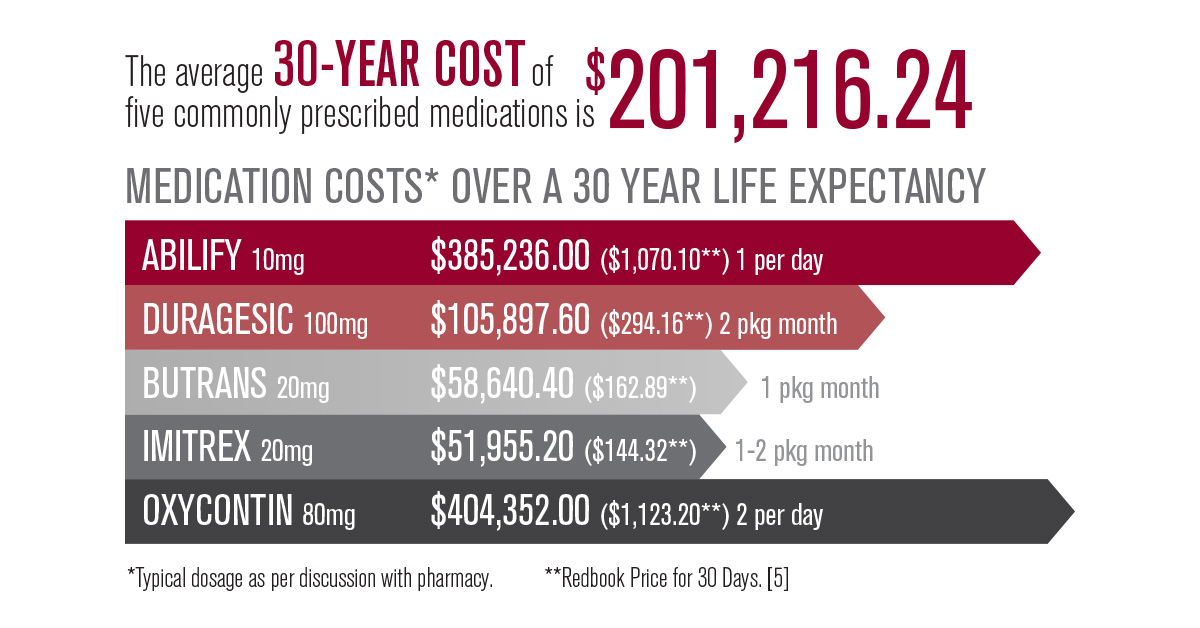
Prescription medications account for an estimated 14% of the total medical costs for workers’ compensation claims, according to the National Council on Compensation Insurance (NCCI), and this estimate has been rising over the last several years [1]. This translates to an estimated $5 billion annually in pharmacy drug costs nationwide. Medication costs for claims older than 11 years can reach as high as 40%. Reviewing medication costs can be one of the most effective ways to control the high cost of workers’ compensation claims. Pharmacists and Pharmacy Benefit Managers (PBM’s) have programs to identify and implement safer and more cost-effective alternatives. After more suitable alternatives have been identified by the pharmacist, the findings are then best communicated to the physician through a consultation with a nurse case manager.
MEDICATION COSTS KEEP RISING IN THE WORKERS’ COMPENSATION INDUSTRY
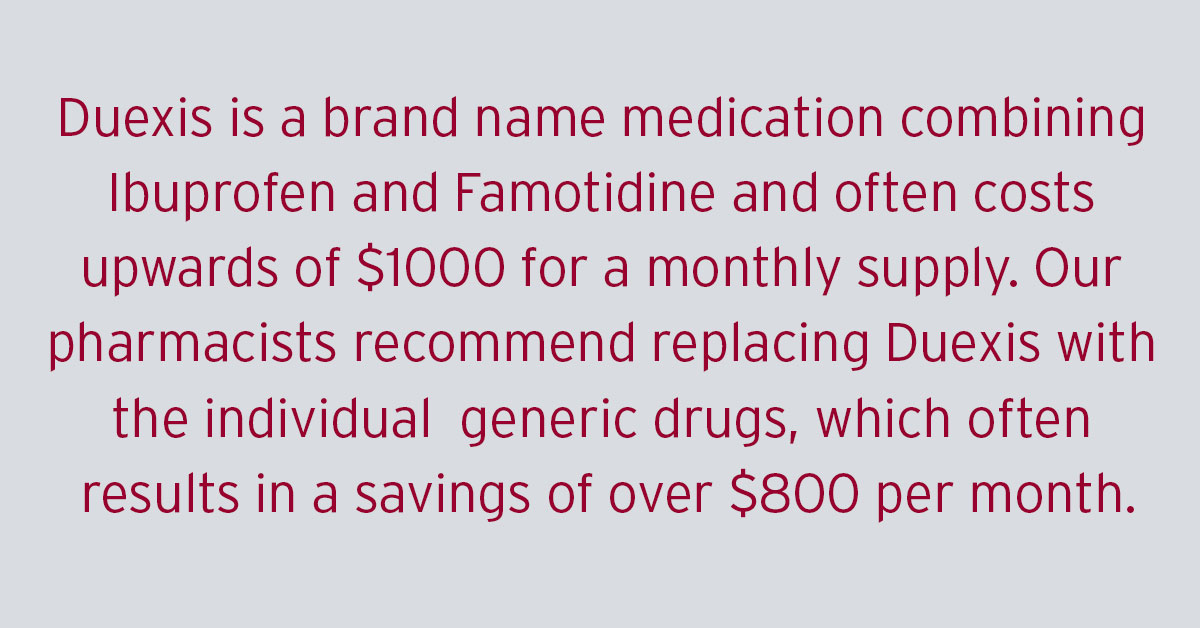
Workers’ compensation medicine and medical costs have increased an average of 4-6% each year, according to an NCCI 2013 study [2]. The major contributors to these costs include: physician dispensing,
utilization of brand name medications, high prices for compounds, specialty medication and rising generic drug costs. In 2011, physician dispensing represented 17% of the total workers’ compensation drug costs, according to the NCCI. Drugs commonly dispensed by physicians cost 60% to 300% more than those dispensed at retail pharmacies, according to the Workers’ Compensation Research Institute. Given these extreme market factors, a collaborative utilization approach by PBM’s and health care professionals can effectively keep costs under control.
PHARMACIST-PROVIDED PRESCRIPTION REVIEWS DRIVE EFFECTIVE MANAGEMENT
Prescription reviews consist of tracking and studying patient data to determine cost-effective alternatives to improve health care outcomes overall. Pharmacists are trained to ensure that the medications prescribed are safe, appropriate and necessary to treat the injury, while restoring the health and productivity of the claimant. Pharmacists and PBM’s understand that appropriate treatment can be reached while reducing medication costs.
Prescription review opportunities can be identified through adjuster requests, pharmacist intervention or internal red flag reporting by a Pharmacy Benefit Manager.
- Has the treating physician(s) failed to respond to inquiries?
- Does the claimant’s monthly medication cost exceed $500?
- Is the claimant prescribed brand name medications that have a generic equivalent?
- Is the claimant prescribed two or more medications in the same therapeutic class?
- Is the claimant prescribed medication that may be unrelated to his/her injury?
- Is this a Medical Only file that has been open for over five years?
- Is the claim approaching settlement? Is an MSA being arranged for this claimant?
- Are there two or more treating physicians on this claim?
- Has the claimant had one or more inconsistent drug screens?
Pharmacist-provided prescription reviews examine the relatedness of treatment to the injury and medication history for the claimant over the prior 90 days. Utilizing patient-specific factors, as well as manufacturer guidelines, retrospective reviews can help identify potential drug-related problems to the claimant including:
- Inappropriate dosage, based on manufacturer guidelines
- Therapeutic duplication (use of multiple drugs from the same therapeutic drug class)
- Excessive duration for prescription drug products
- Drug-disease advisory
- Compound ingredient analysis
- Drug to drug interactions
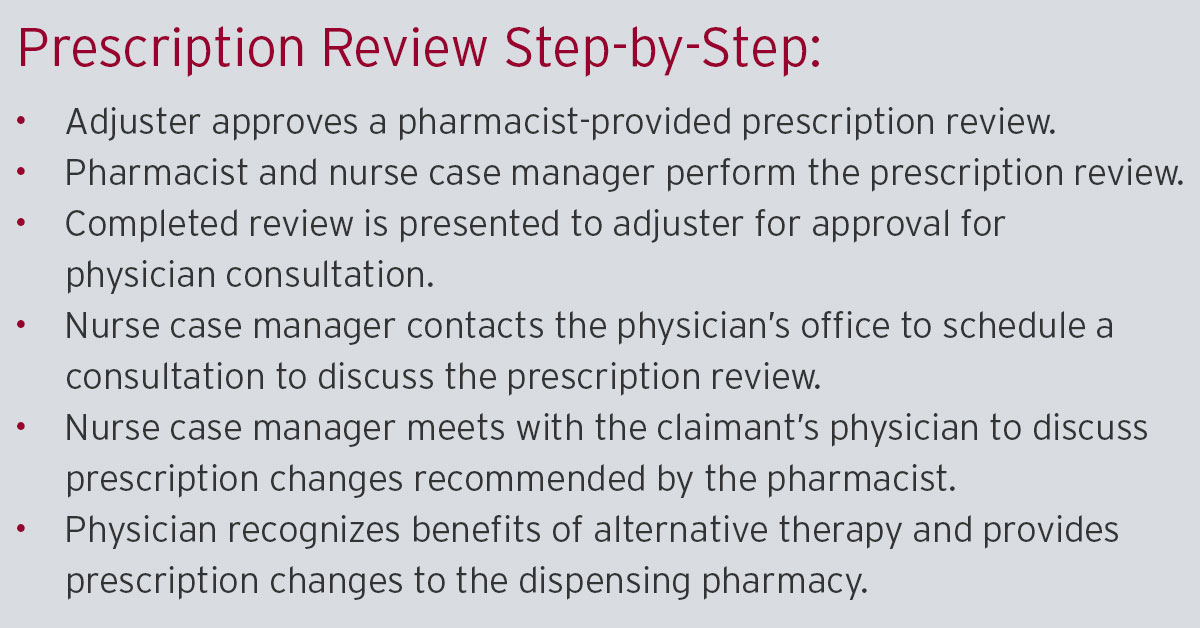
Once the pharmacist identifies a problem, the prescription review will be presented to the physician, providing evidence-supported recommendations for positive changes to the claimant’s current drug therapy. National studies support the helpful impact that pharmacists can have on decreasing unnecessary medication use and total costs. [3] The nurse case manager plays a critical role in the process, by then effectively communicating the proposed changes to the prescribing physician.
[Drug and pharmacy expenses comprise 14% of the average workers’ compensation case file. Many times, employers are asked to cover medical expenses for the life of the patient. ]
It is important to note that prescription reviews do not impact the treatment. Patients are receiving the same treatment with only minor changes in the medication.
> Medicare Set-Asides and Life Care Plans should have Prescription Reviews completed.
COMMUNICATION BY A NURSE CASE MANAGER IS CRITICAL
Typically, nurse case managers are involved with catastrophic claims where there are many details to coordinate between the claimant, employer and physician. However, in recent years it has become clear that nurse participation is vital for successful outcomes. Nurses are now being utilized on all types of claims, including those involving a lesser degree of trauma. With nurse case managers working only 10% of all claims in the workers’ compensation industry, one could make a case that they are being highly underutilized. The goal, however, remains the same; to design, implement and monitor an effective and efficient schema of post-acute care.
Let us define the role of a workers’ compensation nurse case manager by looking at the accepted definition of case management:
Case management is a collaborative process of assessment, planning and
advocacy for options and services to meet an individual’s health needs through
communication and available resources to promote quality, cost-effective
outcomes [4].
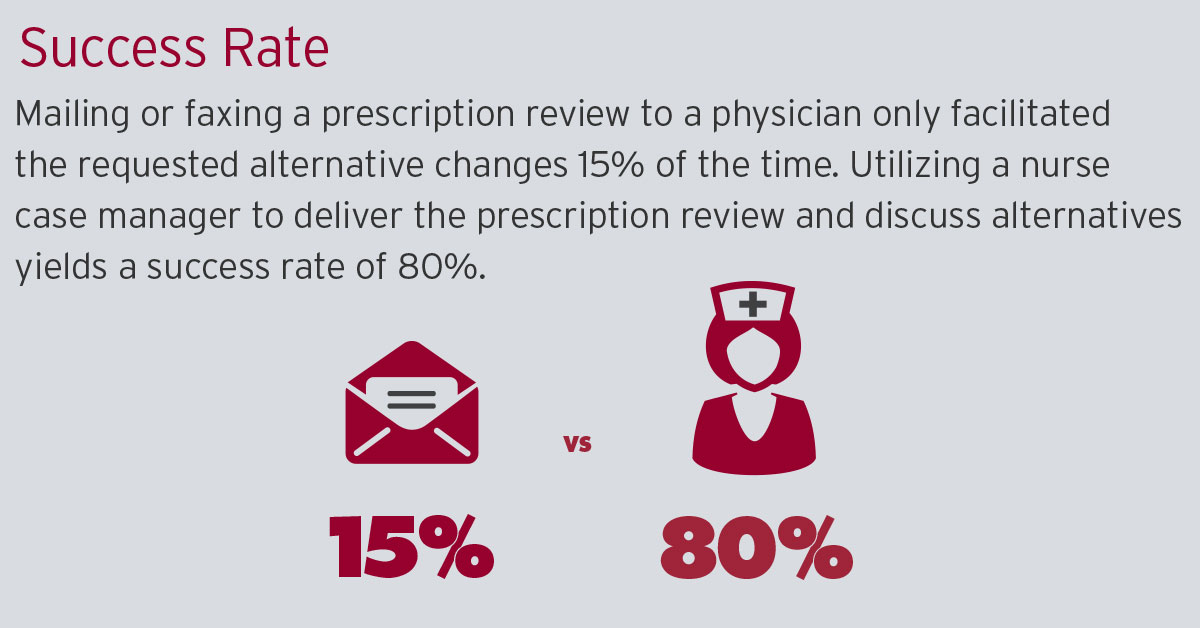
The prescription review/task assignments are a more specific utilization of a nurse case manager’s skills. The pharmacist-provided prescription review and the treatment alternatives are discussed between the pharmacist and nurse, so these changes can be effectively communicated to the physician during the task assignment. The communication between the nurse, physician and claimant facilitates a much more successful outcome than the passive mailing or faxing of a prescription review directly to the physician’s office. Historical tracking by Carlisle Medical shows that the mailing or faxing of a prescription review to a physician only facilitated the requested alternative changes 15% of the time. In contrast, utilizing a nurse case manager to deliver the prescription review and discuss alternatives yields a success rate of 80%. The reasons for increased success can be attributed to a few key points:
- Information is provided clearly and concisely, and the physician is provided the opportunity to have questions answered immediately by the consulting nurse, as it relates to the claimant’s prescription history and suggested alternatives.
- The physician can conveniently write the new prescriptions to make the suggested changes during the consultation.
- The nurse can also facilitate the delivery of the prescription changes to the dispensing pharmacy so changes can be immediate.
CONCLUSION
Companies can gain a positive return on investment from these types of prescription reviews and consultations. In our experience, many companies have the potential to save millions of dollars by partnering with an experienced PBM that is consistently reviewing drug prescription costs and their relation to the claimant’s medical needs. Prescription drug costs will likely continue to escalate for the foreseeable future. Employers and administrators can help contain these costs and drive better
overall workers’ compensation claim outcomes.
INTERNAL EDUCATION
Healthcare professionals can further alleviate rising drug costs by educating adjusters, case managers and risk management resources personnel on prescription review services. Educating claimants about costly treatment can be helpful. Behavioral research has demonstrated that claimants care about the cost of the treatments they receive, including physician-dispensed medication.
CASE STUDY: “A SINGLE PRESCRIPTION REVIEW SAVED $1.7MILLION”
CASE RESULTS
Carlisle Medical was contacted to review a case submitted for an MSA settlement. This particular file was inherited by the client due to a recent company acquisition with an insurance company, which is a common scenario. A 62-year-old patient had hurt his back in a work-related injury. Over the years, he had also hurt his foot, which was not a work-related injury. Although the two injuries were not related, the patient’s doctor was providing care for both injuries. Both injuries utilize the same medication types for treatment, resulting in the continued payment of medications unknowingly.
CASE SYNOPSIS
Carlisle Medical reviewed the case and immediately identified cost savings on the claim. Carlisle Medical found a much more cost-effective treatment planvfor the back injury utilizing therapeutic equivalent prescriptions, thus drastically decreasing the cost of the claim that was about to settle. After revealing their findings to the client, Carlisle Medical immediately scheduled a consult with the physician. During the nurse’s consult with the physician, it was determined that a number of medications the insurance company was paying for were unrelated to the injury. The insurance company was not aware of the foot injury treatment and that the medications prescribed for it would have been included in the settlement. Carlisle Medical recommended generic alternatives for the prescriptions and worked with the doctor and medical staff to isolate the claim only to the original back injury. “It’s almost like playing detective where we have to go back, talk to all parties involved and connect the dots,” said Carlisle. Because this particular case was for a lifetime claim, Carlisle Medical ultimately saved the client $1.7 million dollars on the claim.
*This is an actual case and numerous others have been documented. Saving rates vary, depending on specifics of the claim.
ADDITIONAL RESOURCES:
This white paper was prepared by Carlisle Medical in collaboration with staff pharmacist Heidi Dufrene, Pharm.D. Carlisle Medical has more than 35 years of experience as a leader in healthcare cost containment to the workers’ compensation industry. Our company assists insurance carriers, third-party administrators and employers to significantly reduce their workers’ compensation costs. Our experienced staff of licensed pharmacists and nurses can assist companies with injuries ranging from minor to catastrophic.
REFERENCES
[1] Arnautovic, Nedzad. A Balancing Act: Rx Costs for Workers Comp Claims Prescription Drug Prices Up, But Usage Down. Retrieved 6 February 2023 from https://www.ncci.com/Articles/Pages/Insights-Prescription-Costs-WC-Claims.aspx.
[2] Lipton, Barry, Chris Laws, and Linda Li. August 2011. “Workers Compensation Prescription Drug Study: 2011 Update.” NCCI.
[3] Dole, E. J., Murawski, M. M., Adolphe, A. B., Aragon, F. D., & Hochstadt, B. (2007). Provision of pain management by a pharmacist with prescribing authority. American Journal of Health System Pharmacy.
[4] Case Management Society of America, www.cmsa.org
[5] Actual prescription costs are for generic drugs, when applicable, and were procured using AWP Redbook values.